Over the Threshold: Street Medicine
|
Medical Student Variety Show Supports Chicago Street Medicine
|
Rylie O’Meara: Chicago’s warming shelters are not adequately caring for the unhoused in winter
|
“Most Chicagoans can identify that feeling of relief upon entering a warm building after walking through the bitter cold. It's time we show compassion to our unhoused neighbors and prioritize the creation of reliable and easily accessible warm spaces for all.” Read more...
|
|
“Izquierdo took what she learned from being part of Chicago Street Medicine, an initiative that began in 2016 with several UIC students and a UIC resident physician providing medical attention to people experiencing homelessness. 'I really like the model of bringing medical care in a mobile way to meet people where they’re at,' Izquierdo said.” Read more...
|
UIC medical students, doctors provide migrant care
|
Homeless Americans Are Costing Us Millions Each Year. Street Medicine Would Help
|
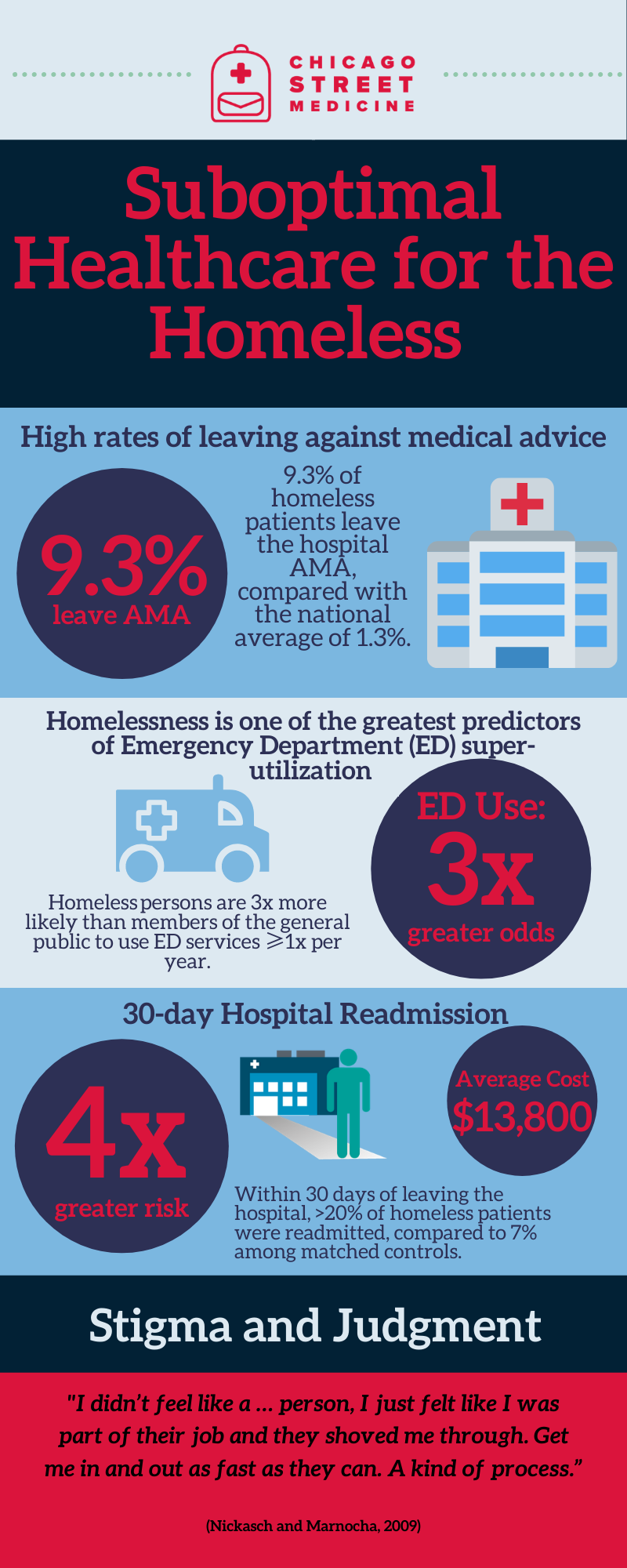
Time and again, people experiencing homelessness have sought care and left feeling humiliated and angry. One man I spoke with equated being in the hospital to animal cruelty—he felt like "a pig in a stall" because he was homeless. Bringing health care workers out on the street can rebuild some of the lost trust felt by some outside of a traditional health care environment. Read more...
|
|
“Through this project, Khan began learning more about addiction and injection drug use, and he began to notice a gap in providers’ understanding of addiction, which affected how his street medicine patients got treated in the hospital, especially in the emergency room.” Read more...
|
Hospital Withdrawal
|
UIC Medical Students Get Healthcare to the Chicago Homeless
|
|
“You can’t just try to fix the medical problem without fixing the social problem that caused the medical problem to happen in the first place.” Read more...
|
UIC Medical Students Seek to ‘Fill a Void’ in Health Care
|
|
| ||||||||||||
International Street Medicine Symposium 2023 Annual Meeting, London UK
Assessing Capacity on the Streets (2018)
|
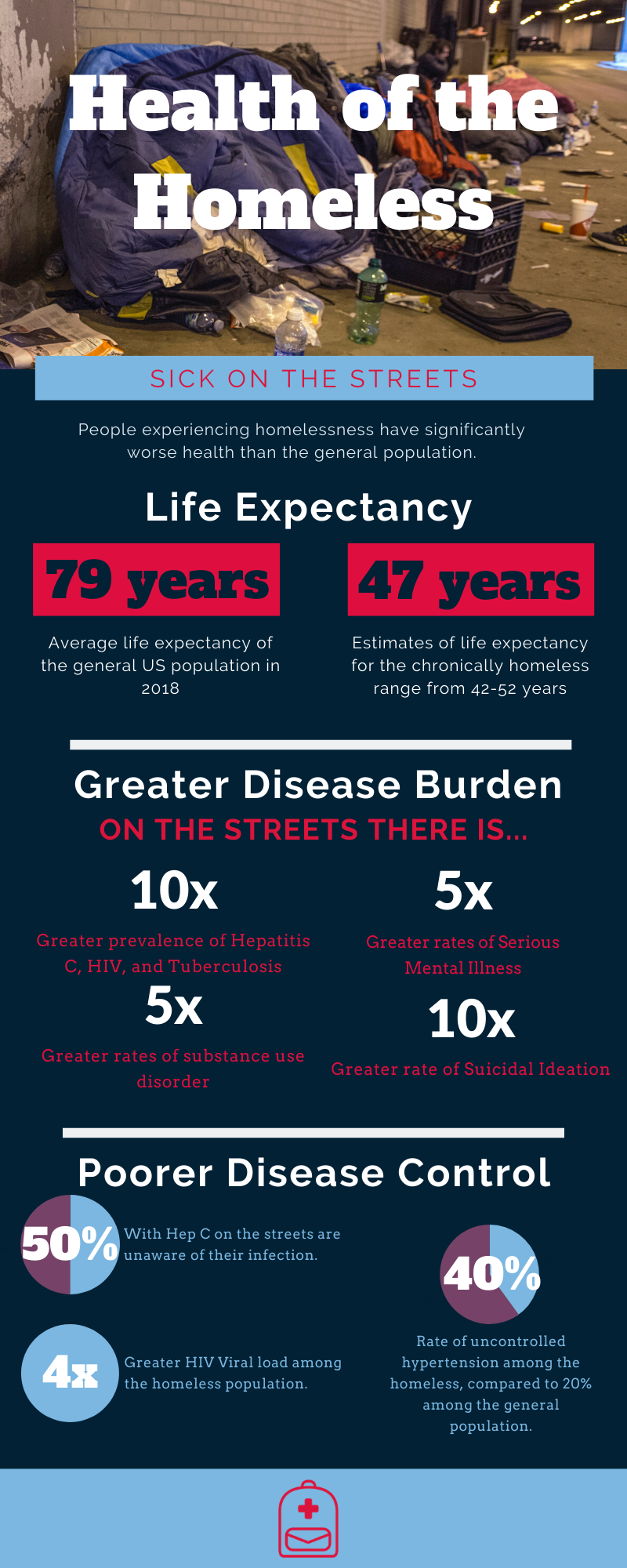
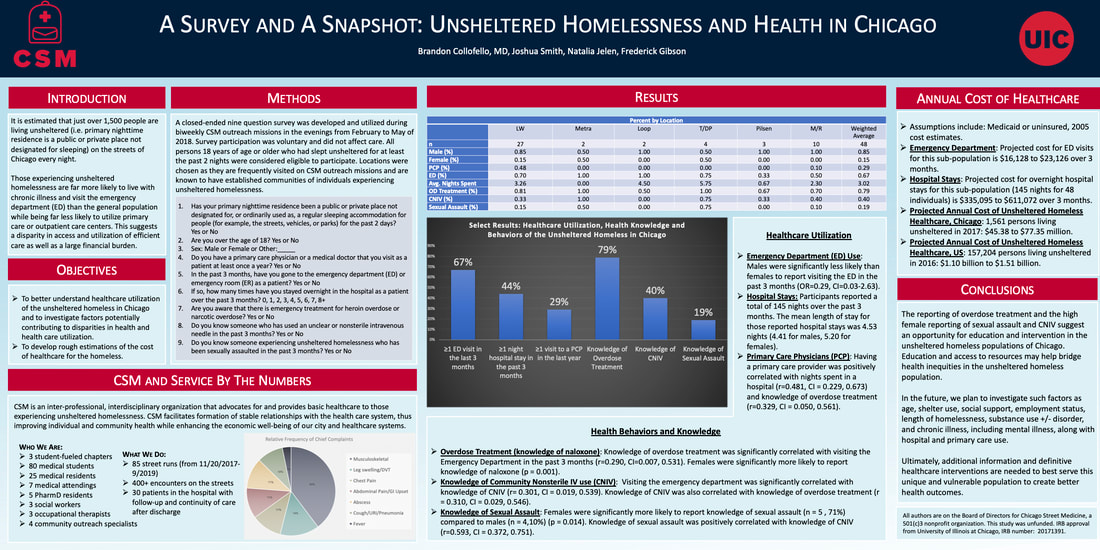
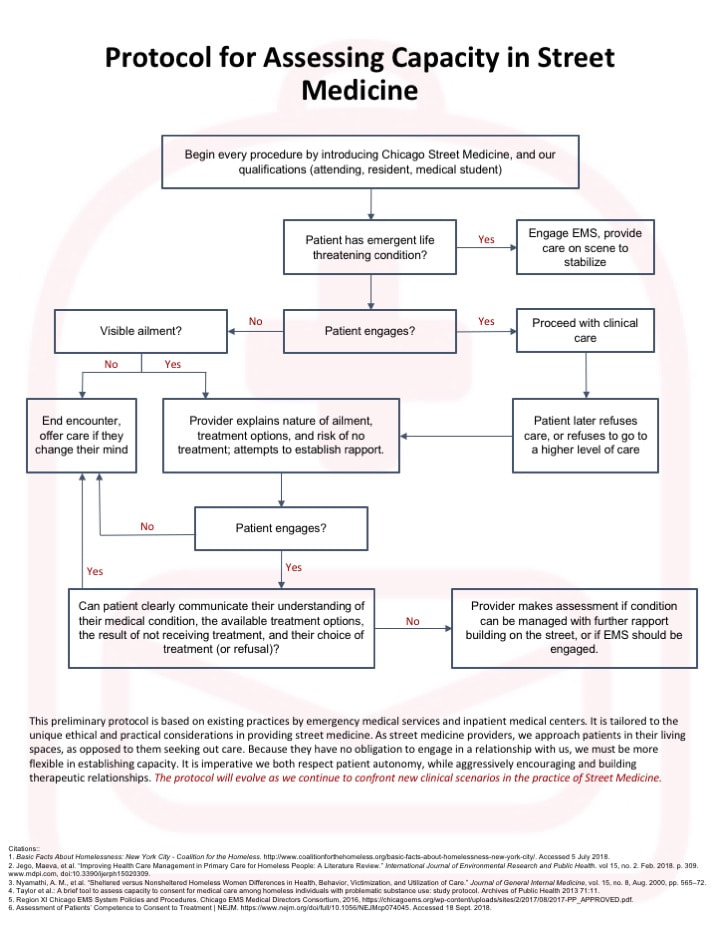
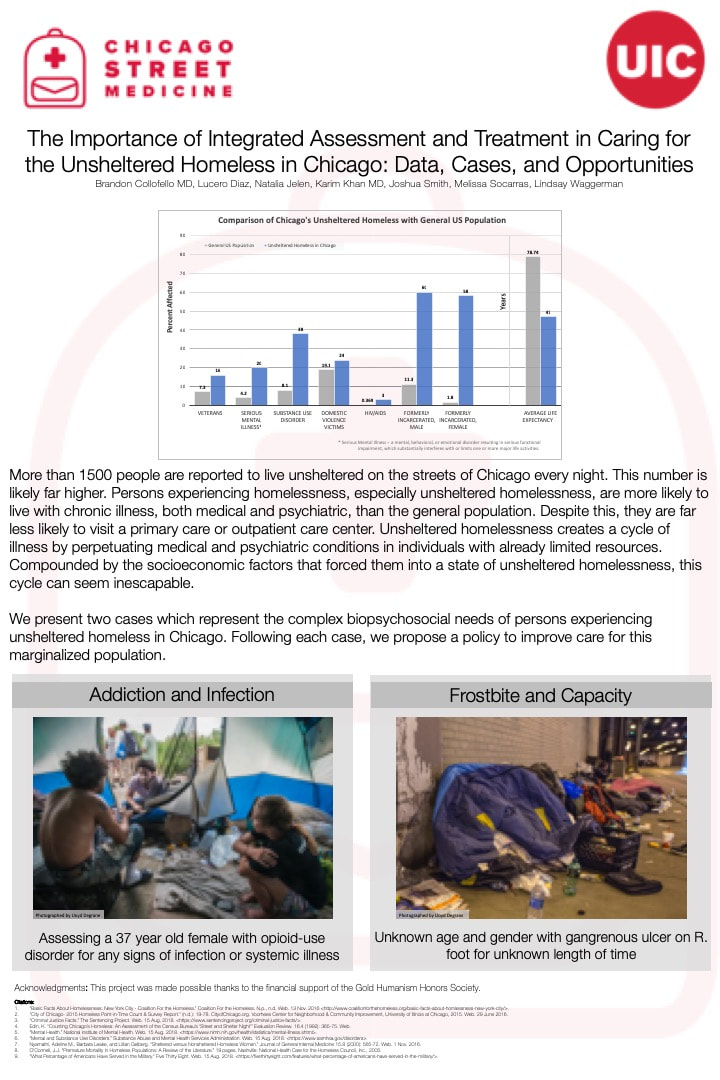
What is the Issue? There is currently no protocol for the assessment of capacity when practicing Street Medicine. Ethical Considerations: Street Medicine organizations work to address the health and social service concerns of the unsheltered homeless by engaging individuals in their spaces of residence and gathering. This population consists of marginalized and vulnerable individuals, who despite living with more chronic illness than the general population, are less likely to utilize primary care or outpatient care services. Additionally, this group is disproportionately affected by mental illness and substance use disorders. As such, caring for these patients and assessing capacity can be very complex. Persons experiencing homelessness, especially those with mental health disorders, are generally assumed to have diminished capacity, thus making them increasingly vulnerable to exploitation and manipulation.4 Therefore, it is important to facilitate trust and to only escalate care against protest when medically appropriate. |
| ||||||
Our Aim:
Many studies have highlighted the increased complexity of assessing decision-making capacity among individuals experiencing homelessness. However, no official protocols have been developed to address the complex needs of the population to ensure that appropriate medical care is given in a respectful manner. As such, our aim is to propose a streamlined protocol which could be used by street medicine practitioners to enhance the ability of providers to assess capacity and thus deliver higher quality health care.
Existing Protocols:
Chicago EMS Protocol
When an adult patient who is alert, oriented, and able to communicate refuses care or transportation, it is the responsibility of the EMS provider to advise the patient of his/her medical condition and explain the necessity for care or transport. If the patient continues to express steadfast refusal, online medical control should be contacted while on scene, and all events should be documented.
Alternatively, if the patient demonstrates behavior and/or has a medical condition that impairs decision making capacity, EMS should continue treatment and transport in the best interest of patient. Patient capacity may be impaired in trauma, intoxication, hypoxia, dementia, and psychiatric or behavioral emergencies, including suicidality and inability to care for self.
Inpatient Protocol
Clinicians often have to assess for capacity while treating patients in an inpatient setting. The main principles guiding capacity assessment include obtaining informed consent prior to initiating treatment and ensuring that patients are able to make informed decisions for themselves. There are many tools to assess mental capacity including the Mini Mental Status Exam and MacArthur Competence Assessment Tool for Treatment. To demonstrate capacity, patients and clinicians must work together to establish that patients can:
Many studies have highlighted the increased complexity of assessing decision-making capacity among individuals experiencing homelessness. However, no official protocols have been developed to address the complex needs of the population to ensure that appropriate medical care is given in a respectful manner. As such, our aim is to propose a streamlined protocol which could be used by street medicine practitioners to enhance the ability of providers to assess capacity and thus deliver higher quality health care.
Existing Protocols:
Chicago EMS Protocol
When an adult patient who is alert, oriented, and able to communicate refuses care or transportation, it is the responsibility of the EMS provider to advise the patient of his/her medical condition and explain the necessity for care or transport. If the patient continues to express steadfast refusal, online medical control should be contacted while on scene, and all events should be documented.
Alternatively, if the patient demonstrates behavior and/or has a medical condition that impairs decision making capacity, EMS should continue treatment and transport in the best interest of patient. Patient capacity may be impaired in trauma, intoxication, hypoxia, dementia, and psychiatric or behavioral emergencies, including suicidality and inability to care for self.
Inpatient Protocol
Clinicians often have to assess for capacity while treating patients in an inpatient setting. The main principles guiding capacity assessment include obtaining informed consent prior to initiating treatment and ensuring that patients are able to make informed decisions for themselves. There are many tools to assess mental capacity including the Mini Mental Status Exam and MacArthur Competence Assessment Tool for Treatment. To demonstrate capacity, patients and clinicians must work together to establish that patients can:
- Clearly communicate their understanding of their medical condition
- Clearly communicate the available treatment options
- Clearly communicate the result of not receiving treatment
- Clearly communicate their choice of treatment (or refusal of treatment)
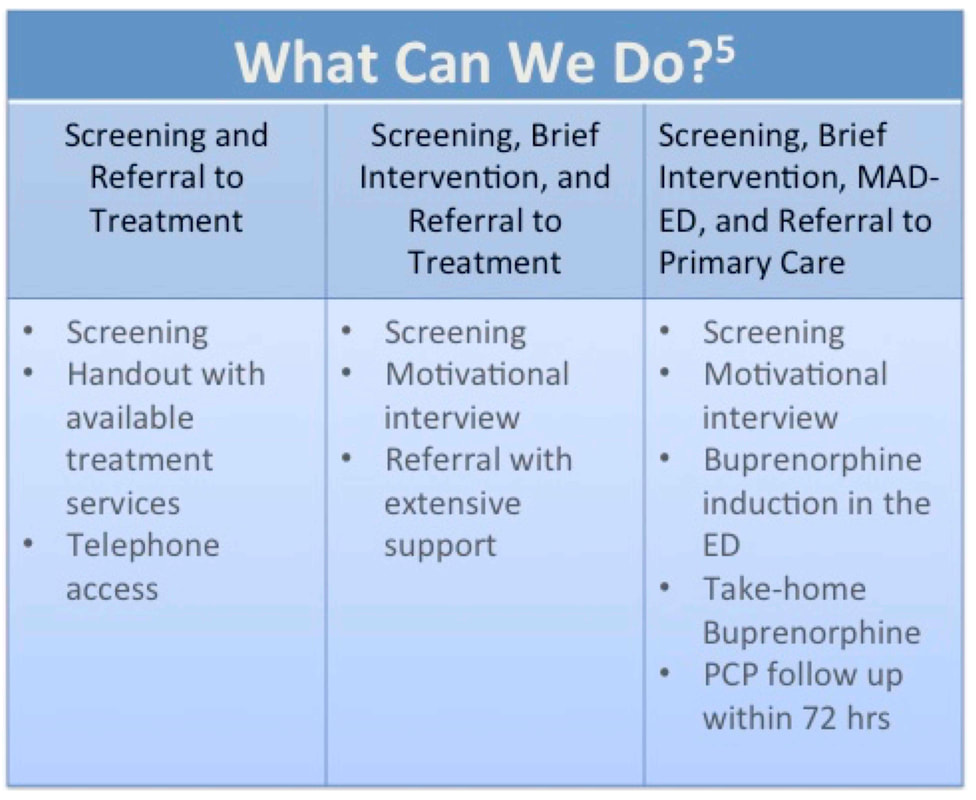
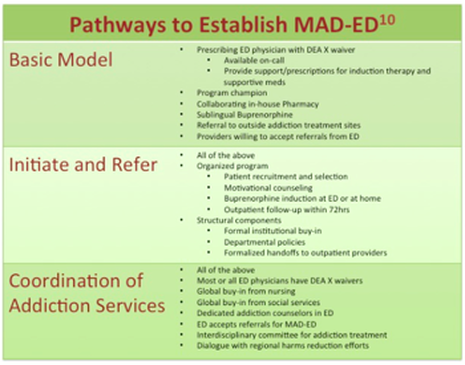
Medication assisted Detoxification in the Emergency Department (MAD-ED): A Policy Proposal for Safety Net Hospitals (2018)
What is the issue?
There is currently no protocol for initiating Medication-Assisted Detox in the Emergency Department (MAD-ED) in safety-net hospitals in Chicago
Why is this is an issue?
Patients suffering from opioid-use disorder have very complex medical needs that are not currently being addressed. Chronic drug users utilize 30% more emergency healthcare services than the general population and are at higher risk for hospitalization, but due to fears of withdrawal and stigmatization, these patients frequently delay care and leave AMA far more often than the general population. This leads to increased costs for their care and increased morbidity and mortality after hospitalization.
There is currently no protocol for initiating Medication-Assisted Detox in the Emergency Department (MAD-ED) in safety-net hospitals in Chicago
Why is this is an issue?
Patients suffering from opioid-use disorder have very complex medical needs that are not currently being addressed. Chronic drug users utilize 30% more emergency healthcare services than the general population and are at higher risk for hospitalization, but due to fears of withdrawal and stigmatization, these patients frequently delay care and leave AMA far more often than the general population. This leads to increased costs for their care and increased morbidity and mortality after hospitalization.
|
Key Further Reading
|
Data to support
When compared to Screening and Referral (with or without Brief Interventions), initiating medication assisted treatment in the emergency department was significantly more effective in:
Establish a Medication Assisted Detox in the Emergency Department (MAD-ED) in Chicago’s safety-net hospitals
| ||||||
The Street Medicine program... has reduced 30-day readmission rates to Lehigh Valley Hospital from 51 percent to 13 percent.. [and has raised] the rate of insured homeless from 24 percent to 73 percent |
For hospital both private and public, recuperative care also has the potential to lower overall costs and decease the rate of hospital readmissions. Health officials estimate that each day in a bad at LA County's safety-net hospital costs the county more than $3,000, while a bed at a recuperative care facility averages about $150 per day |
The only difference between the homeless women I regularly hear from and the women who are now coming forward and having their stories believed is that when homeless women speak, no one listens... women experiencing homelessness already live at the margins of society. in the margins of society, in the margins of the MeToo Movement, and in the margins of our minds. At the very least, we must see and acknowledge their reality |
"MILLION DOLLAR MURRAY"
|
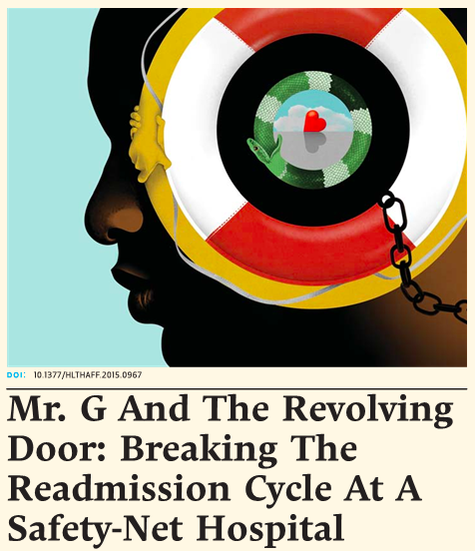
"MR. G AND THE REVOLVING DOOR"
"A patient with complex needs returns to the hospital again and again, despite his care team's efforts to reduce readmissions"
~Carolyn Dickens, Denise Weitzel, and Stephen Brown Read more... |
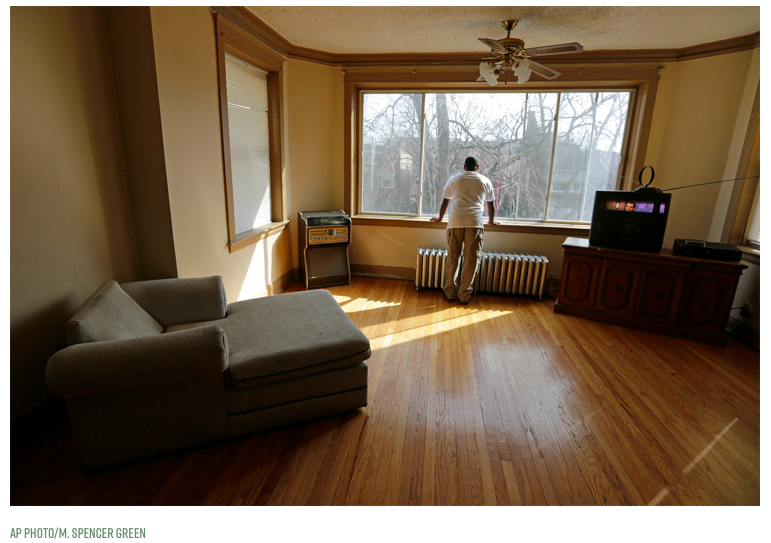
"Opportunity starts at home. our advocacy starts now."
"Articulate the goal and the broad strategy for achieving it...identify and work with all parties affected...set specific objectives...organize all the related interests in support of those objectives."
Read more... |